New economic model finds Fracture Liaison Services are highly effective
The newly developed model to estimate the health benefits and budget impact of Fracture Liaison Services (FLS) is an important tool to drive the prioritisation of FLS provision within healthcare systems.
New research reveals that widespread Fracture Liaison Service (FLS) implementation would benefit patient outcomes, manifested in a significant reduction in subsequent fragility fractures and gains in quality of life, whilst at the same time reducing hospital bed days, surgeries, need for institutional social care, and their associated costs.
With populations ageing, the burden of fragility fractures on healthcare systems around the world is on the rise, resulting in a spiral of increased patient disability, loss of independence, and early mortality within the older population. Given that patients with a fragility fracture are at substantially high risk of subsequent fractures, effective secondary fracture prevention is of critical importance. In this regard, Fracture Liaison Services (FLS) have been shown to be an optimal way to systematically identify, assess, treat, and monitor patients who have recently sustained a fragility fracture, and they have been proven to reduce the risk of subsequent fractures in numerous studies and reviews.
Associate Professor Kassim Javaid, Lecturer in Metabolic Bone Disease and Honorary Consultant Rheumatologist, NDORMS, University of Oxford, UK, co-author of the study, stated:
“Although FLSs are highly effective in reducing the risk of subsequent fragility fractures and improving patient outcomes, the majority of healthcare settings that manage adult fracture patients do not have an FLS in place. In the European Union for example, 50% of countries reported FLS coverage in less than 10% of hospitals. We know that a major barrier to sustainable effective FLS implementation is a lack of national, regional, and local policy prioritisation and reimbursement. This new model makes visible both the invisible costs of fragility fracture and the expected net benefits from systematic FLS provision to patients and their family, clinicians, healthcare systems, and wider society. The flexibility of the model allows its implementation across different types of healthcare systems and populations and provides clear outputs tailored to a wide audience, giving decision makers critical information based on their local data to appropriately prioritise local implementation of FLS for patient benefit.”
The microsimulation model estimates the impact of FLSs compared to current practice for men and women 50 years of age or older with a fragility fracture. It provides estimates for health outcomes that include subsequent fractures avoided and quality-adjusted life years (QALYs), as well as resource use, and health and social care costs, including those necessary for FLSs to operate, over five years.
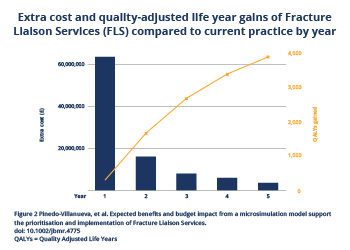
Based on an exemplar country the size of the United Kingdom, FLSs were estimated to lead to a reduction of 13,149 subsequent fractures and a gain of 11,709 QALYs over the first five years of FLS implementation. Hospital bed days would be reduced by 120,989 and surgeries by 6,455, whilst 3,556 person-years of institutional social care would be avoided. Expected costs per QALY gained placed FLSs as highly cost-effective at £8,258 per QALY gained over the first five years alone.
Associate Professor Rafael Pinedo-Villanueva, Senior Health Economist, NDORMS, University of Oxford, first author of the study, explains:
“With healthcare budgets being limited and increased pressures on healthcare providers, policy makers need to make informed decisions based not only on necessary investments but also on expected benefit to patients, impact on healthcare resource use, and cost impacts before they can prioritise secondary fracture prevention in relation to other health priorities. This model acts as a calculator for all these relevant outcomes and can be run for any country or region. When run with values for a country the size of the United Kingdom, it shows that the initial investment in FLS implementation, where extra costs are concentrated in the first year, is worthwhile. The costs then drop significantly thereafter as we see gains in QALYs over time as more and more fractures are avoided.”
“Further work to develop country-specific models is currently underway, and we expect that this will deliver crucial national level data that can then be used to inform policy makers at the country level.”
The development of the model was carried out by experts from the University of Oxford and supported by the International Osteoporosis Foundation (IOF) Capture the Fracture® initiative, a programme which works to drive the implementation and sustainability of FLS worldwide, and which offers best-practice guidance and recognition to more than 800 FLS in all regions of the world.
Professor Cyrus Cooper, IOF President and co-author, concluded:
“This important model, essentially an ‘FLS cost and benefit’ calculator, provides significant evidence that secondary fracture prevention through FLS service provision is highly cost effective, with significant benefits for patients, their families, the healthcare system, and society as a whole.”
###
Further reading
- Rafael Pinedo-Villanueva, Edward Burn, Christopher Maronga, Cyrus Cooper, M. Kassim Javaid. Expected benefits and budget impact from a microsimulation model support the prioritisation and implementation of Fracture Liaison Services doi: 10.1002/jbmr.4775
- What is a Post-Fracture Care Coordination Program / Fracture Liaison Service
- Policy report: Capture the Fracture® Partnership Guidance for Policy Shaping
About Capture the Fracture®
Capture the Fracture® (CTF) is a multi-stakeholder initiative, led by the International Osteoporosis Foundation (IOF), to facilitate the implementation of Post-Fracture Care (PFC) Coordination Programs, such as Fracture Liaison Services (FLS), for secondary fracture prevention. The CTF initiative, which celebrated its 10th year of service in 2022, aims to drive changes at local and regional levels to prioritize secondary fracture prevention. It sets global best practice standards and offers recognition for Fracture Liaison Services (FLS) through its Best Practice Framework. CTF also provides essential resources and documentation to build the case for prioritization of secondary fracture prevention and to help drive the implementation and quality improvement of FLS. Mentorship programs that support the development of FLS at the local level are also offered.
The Capture the Fracture® Partnership, a global initiative launched in 2020, is a collaboration between the International Osteoporosis Foundation (IOF), the University of Oxford, Amgen and UCB, amplifying the Capture the Fracture programme launched in 2012. It seeks to address the global health burden of osteoporosis through five interconnected pillars, following a comprehensive, top-down and bottom-up approach, and aligning stakeholders at the international, national and local level in prioritized countries across the Asia Pacific, Europe, Latin America and the Middle East. The aim is to prioritize PFC and drive more rapid uptake of PFC coordination programs around the world.
Currently, the CTF network includes 812 FLS in 53 countries worldwide. FLS are invited to apply for free assessment and recognition via the CTF website’s online Best Practice Framework application platform. https://www.capturethefracture.org #CaptureTheFracture
About IOF
The International Osteoporosis Foundation (IOF) is the world's largest nongovernmental organization dedicated to the prevention, diagnosis, and treatment of osteoporosis and related musculoskeletal diseases. IOF members, including committees of scientific researchers as well as more than 300 patient, medical and research organizations, work together to make fracture prevention and healthy mobility a worldwide heath care priority. https://www.osteoporosis.foundation @iofbonehealth
About the Nuffield Department of Orthopaedics, Rheumatology and Musculoskeletal Sciences (NDORMS)
The Nuffield Department of Orthopaedics, Rheumatology and Musculoskeletal Sciences (NDORMS) is a multi-disciplinary department focusing on discovering the causes of musculoskeletal and inflammatory conditions to deliver excellent and innovative care that improves people’s quality of life. The largest European academic department in its field, NDORMS is part of the Medical Sciences Division of the University of Oxford, and is a rapidly growing community of more than 500 orthopaedic surgeons, rheumatologists and scientists all working in the field of musculoskeletal disorders.
The research work of the department takes place in several locations across the Nuffield Orthopaedic Centre, namely the Botnar Institute for Musculoskeletal Sciences, the Kennedy Institute of Rheumatology, and the Kadoorie Centre. The co-location with NHS services puts the department in an excellent position with basic researchers working alongside clinicians. This substantially improves research capacity, improving access for researchers to patients, and facilitating the interaction between clinicians and scientists that is essential for successful medical research.
https://www.ndorms.ox.ac.uk/