What is a Post Fracture Care Coordination Program (PFC) ?
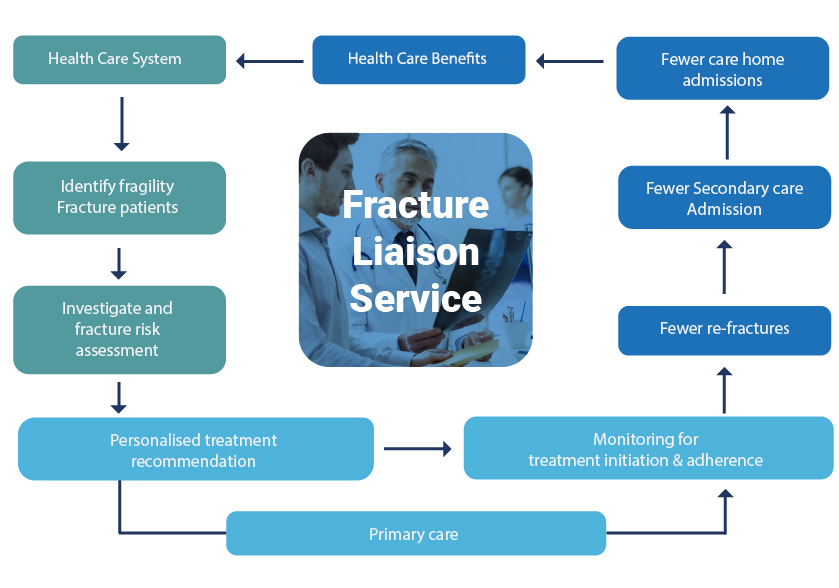
Post-Fracture Care (PFC) Coordination Programs, such as Fracture Liaison Services (FLS), are coordinator-based, secondary fracture prevention services implemented by health care systems for the treatment of osteoporotic patients.
PFC Coordination Programs are designed to: Close the care gap for fracture patients 80% of whom are currently never offered screening and/or treatment for osteoporosis Enhance communication between health care providers by providing a care pathway for the treatment of fragility fracture patients
PFC Coordination Program Structure
PFC Coordination Programs, most commonly known as FLS, are made up of a committed team of stakeholders, employing a dedicated coordinator to act as the link between the patient and the orthopaedic team, the osteoporosis and falls prevention services, and the primary care physician.
An FLS ensures that all patients presenting with fragility fractures to the locality or institution receive fracture risk assessment and treatment where appropriate. The service is comprised of a dedicated case worker, often a clinical nurse specialist, who works to pre-agreed protocols to case-find and assess fracture patients. The FLS can be based in secondary or primary care health care settings and requires support from a medically qualified practitioner, whether it be a hospital doctor with expertise in fragility fracture prevention or a primary care physician with a specialist interest.
The service structure for a UK hospital-based Fracture Liaison Service is illustrated below.
Economic benefits of PFC
In the prevailing global economic climate, robust demonstration of cost-effectiveness is a prerequisite if new models of care are to be broadly implemented. In a growing number of countries throughout the world, PFC Coordination Programs have been shown to be highly cost-effective for healthcare systems by improving patient care, reducing secondary fracture rates, and ultimately, decreasing the healthcare and societal burden.
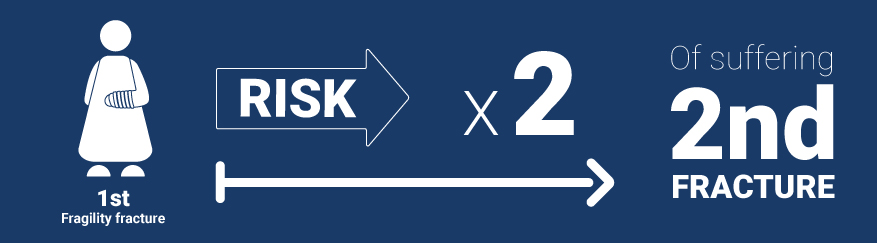
Patients who have suffered a fragility fracture have double the risk of suffering another fracture. By intervening with appropriate diagnosis, treatment and care after the first fracture, we can significantly reduce the number of patients suffering and associated healthcare costs.
A cost-benefit analysis
The Glasgow FLS analysed the cost effectiveness of its FLS over the last 8 years during which they have been providing secondary fracture care in Glasgow, Scotland. From the results, it is estimated that implementing an FLS for the entire UK, it will cost just 0.6% of the current annual hip fracture costs. In summary:
FLS cohort of 686 patients, compared with 'usual care' cohort of 193 patients:
- 18 fewer fractures
- 3 life years gained
- 22 QALYs gained
- 266 hospital bed-days saved
- cost saving of 312 000 GBP (US $497 498) from fractures avoided
| FLS cohort | Usual care cohort | |
|---|---|---|
| Cost of assessments | 98'000 GBP (US $ 156’208) | 14’000 GBP (US $ 22’316) |
| Cost of drugs | 292’000 GBP | 85’000 GBP (US $ 135’535) |
| Overall savings | 21’000 GBP / 1’000 patients (US $33’482) |
Read more about the cost-savings at the Glasgow FLS.
Modelling of the costs of second fractures and the impact of effective FLS are available at national, regional and local levels below.
Health economic publications
Australia
CONCORD REPATRIATION GENERAL HOSPITAL, SYDNEY, NEW SOUTH WALES
Cost-effectiveness of the Concord Minimal Trauma Fracture Liaison service, a prospective, controlled fracture prevention study. Cooper MS, Palmer AJ, Seibel MJ. Osteoporos Int. Jan 2012;23(1):97-107. PubMed ID 21953475
Canada
EDMONTON HOSPITALS, ALBERTA
Osteoporosis case manager for patients with hip fractures: results of a cost-effectiveness analysis conducted alongside a randomized trial.. Majumdar SR, Lier DA, Beaupre LA, Hanley DA, Maksymowych WP, Juby AG, Bell NR, Morrish DW. Arch Intern Med. 2009 Jan 12;169(1):25-31. PubMed ID 19139320
ST. MICHAEL’S HOSPITAL, TORONTO, ONTARIO
A coordinator program in post-fracture osteoporosis management improves outcomes and saves costs. Sander B, Elliot-Gibson V, Beaton DE, Bogoch ER, Maetzel A. J Bone Joint Surg Am. Jun 2008;90(6):1197-1205. PubMed ID 18519311
Italy
Pharmacological treatment of hip fractured patients in Italy: a simulation based on Tuscany regional database for the TARGET project. Piscitelli P, Metozzi A, Brandi ML, Nuti R, Rizzuti C, Orlandini E, Giorni L, Merlotti D. Clin Cases Miner Bone Metab. 2010 May;7(2):140-143. PubMed ID 22460020
SPAIN
Naranjo A, Prieto-Alhambra D, Sánchez-Martín J, Pérez-Mitru A, Brosa M. Clinicoecon Outcomes Res. 2022 Apr 22;14:249-264. doi: 10.2147/CEOR.S350790. PubMed ID 35492806
UNITED STATES OF AMERICA
Prevalence and costs of osteoporotic patients with subsequent non-vertebral fractures in the US.. Pike CT, Birnbaum HG, Schiller M, Swallow E, Burge RT, Edgell ET. Osteoporos Int. 2011 Oct;22(10):2611-2621. PubMed ID 21107532
Cost burden of second fracture in the US health system. Song X, Shi N, Badamgarav E, Kallich J, Varker H, Lenhart G, Curtis JR. Bone. 2011 Apr 1;48(4):828-836. PubMed ID 21211578
GEISINGER HEALTH SYSTEM, PENNSYLVANIA
Osteoporosis disease management in a rural health care population: hip fracture reduction and reduced costs in postmenopausal women after 5 years. Cooper MS, Palmer AJ, Seibel MJ. Osteoporos Int. Jan 2012;23(1):97-107. PubMed ID 21953475
KAISER PERMANENTE, SOUTHERN CALIFORNIA
Osteoporosis disease management: the role of the orthopaedic surgeon. Dell R, Greene D, Schelkun SR, Williams K. J Bone Joint Surg Am. Nov 2008;90 Suppl 4:188-194. PubMed ID 18984730 PubMed ID 21953475